Do you know what is funny? How people think alcoholic beverages can be taken without caution because most of them seem to be bitter.
So, you see people taking bottles/cans of beer, and shots of spirits at a sitting, feeling it won’t be detrimental to their health.
Our work-hard-party hard kind of lifestyle has made it possible for the risk of hypertension to be increased especially among youths. Hypertension is a lifestyle disease, so we must all be able to look at our lifestyle and make a change to it.
Also, the idea that alcohol is a stress reliever, makes it possible for people to consume without caution which in turn hurts the liver and brain, possibly leading to hypertension
WHAT IS THE LINK BETWEEN ALCOHOL INTAKE AND HYPERTENSION?
Alcohol is one of the modifiable ways to reduce hypertension. The link between alcohol and hypertension is clear as alcohol is a major contributory factor in hypertension
Studies have shown that taking more than three alcoholic drinks a day can increase the chance of developing hypertension in later life by up to 75%.
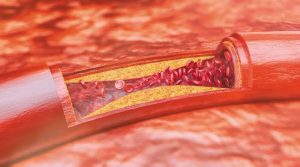
Alcohol has both direct and indirect links to hypertension: It can cause you to gain weight which is linked to hypertension, and it can also directly affect your blood pressure readings.
Furthermore, alcohol may stimulate adrenals which release adrenaline. When adrenaline is released, it leads to increased cardiac output, increased heart rate, and increased systolic blood pressure.
BUT RED WINE IS GOOD FOR MY HEART?
Well, several past studies have made this popular. The idea behind this is that grapes used in making red wine contain reservatol and can help keep the heart and provide other benefits. But truly, the amount of reservatol in red wine is affected by the processing, fermentation, and even aging of wine and cannot be sufficient to provide any heart health benefits as purported.
It is important to pay attention to your lifestyle: quit binge drinking, reduce or stop consumption of alcohol if you’re on blood pressure medications or have a family history, try abstinence!
SOURCES:
– https://www.medanta.org/patient-education-blog/the-truth-about-alcohol-and-hypertension/#:~:text=Drinking%20too%20much%20alcohol%20can,doubles%20the%20risk%20of%20hypertension.
– https://pubmed.ncbi.nlm.nih.gov/18259032/
– https://www.drugsandalcohol.ie/24301/1/Alcohol-and-Hypertension_Factsheet.pdf
– https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4038773/#:~:text=It%20is%20possible%20that%20alcohol,oxidative%20injury%20to%20the%20endothelium.




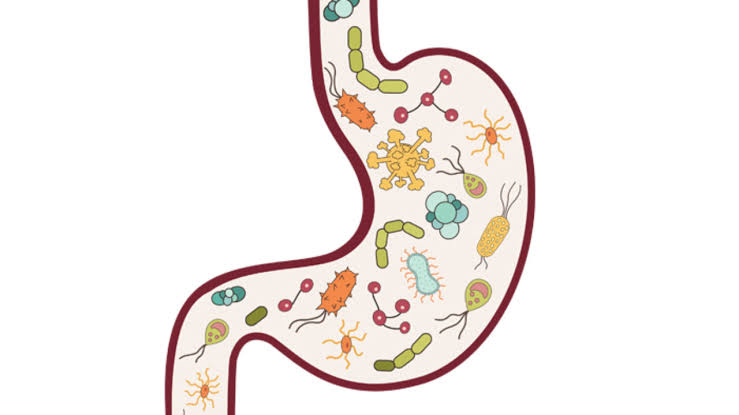
 The talk about gut health and hormones isn’t yet hitting the internet as it should. Rather, everyone is more concerned about their shape and the size of their belly. Your gut and hormones are intrinsically connected and affect your health in ways you can’t imagine.
The talk about gut health and hormones isn’t yet hitting the internet as it should. Rather, everyone is more concerned about their shape and the size of their belly. Your gut and hormones are intrinsically connected and affect your health in ways you can’t imagine.