The earlier we all understand that food and dietary patterns have a way of affecting us emotionally, the better.
If we can be mindful about so many things including what we wear, where we go, who we date etc, then we should also should be able to practise mindfulness not just while selecting ingredients for food or where to eat, but also how to eat.
It sounds quite funny that you’ll have to practise mindfulness when it comes to eating habits, but it is very important as it can help prevent being overweight and also emotional eating which can lead to eating disorders.
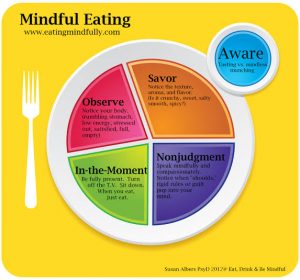
In fact, The term “mindfulness” was defined by Jon Kabat-Zinn as “paying attention in a particular way, on purpose, in the present moment, and nonjudgmentally”.
Mindful eating on its own is a type approach to food that addresses how an individuals senses appeals to food and their experience with that food.
Apart from helping to prevent further weight gain, mindful eating also helps to create a very healthy relationship with food and removes guilt and anxiety that comes with eating for some people.
HERE ARE 7 PRINCIPLES OF MINDFUL EATING
– Honor the food:. Sounds a bit odd, but acknowledging how the food was prepared and who made the food brings to you a sense of belonging.
– Engage all senses: The aroma, taste, hotness or coldness of the food helps you appreciate it more. It also helps to pause at intervals and can reduce overeating.
– Serve in modest portions: portion control is also part of mindful eating. Making sure that every food is served at the right amount cuts out overeating and wastage too.
– Chew thoroughly: These practices can help slow down the meal and fully experience the food’s flavors.
– Eat slowly to avoid overeating: carefully masticating food, can help you realise when you are satisfied. This way, you don’t ignore satiety and go on eating, then feel guilty after the meal.
– Don’t skip meals: mindfulness about food can always get you excited before every meal. You’re always looking forward to every healthy meal and this way, you don’t skip meals at all. The body/brain has a way of playing on you to unintentionally overeat after skipping a meal.
– Observe: notice your body language. Check out when your body gives you signs that it’s full and stop eating. Eat only when you get hunger cues and not when you are sad or overly happy. Be observant.
Practising mindfulness is highly important to improve your relationship with food. Diseases and eating disorders all come from not being mindful about our food choices. Start from today and become mindful and see the wonders of this practise.
SOURCES:
– https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5556586/
– Am I Hungry.com. Mindful eating programs and training [Internet]. Available from http://www.amihungry.com. Accessed 13 January 2017
– Harris C. Mindful eating: studies show this concept can help clients lose weight and better manage chronic disease. Today’s Dietitian 2013;15:42. Available from http://www.todaysdietitian.com/newarchives/030413p42.shtml. Accessed 17 May 2017
– Rossey L. The Mindfulness-Based Eating Solution. Oakland, Calif., New Harbinger Publications, 2016