It is normal to sometimes get things mixed up especially when they seem to share some similarities such as gall stone and kidney stone, chronic acid reflux and ulcer but we would be focusing on these most common two diseases, “gall stone and kidney stones”. 
- So many people actually have gall stone but would mistake it for kidney stone. Well, worry less if you probably fall into this category. This article would help enlighten you more on the differences of both types of stones.
Gall stones or kidney stones are two conditions that could cause excruciating pains to any individual, but some people really don’t know they are both different preventive measures and treatment approaches.
CHARACTERISTICS OF KIDNEY STONES AND GALLSTONES
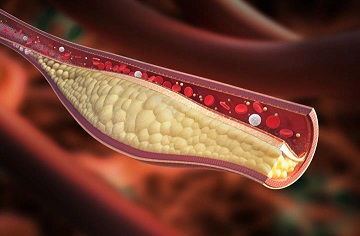
- Gall stones are cholesterol deposits that resemble pebbles, WHILE kidney stones are cement-like and are made of dissolved minerals in the urine
- Gallstones are found inside the gall bladder WHILE kidney stones develop in the urinary tract
SIMILARITIES AND SYMPTOMS OF KIDNEY STONES AND GALLSTONES
- Kidney stones are small as sand grains and grow larger causing pain when you try to urinate WHILE gall stones can be as small as sand grains too and can grow as big as a golf ball
- Kidney stones comes with symptoms like blood in the urine, painful urination, inability to urinate frequently WHILE gall stones come mostly with nausea, vomiting, fever and sweating.
CAUSES KIDNEY STONES AND GALLSTONES
- For kidney stones, foods that are high in sodium, animal protein can increase the risk of developing kidney stones. Foods like processed meat, canned/ tinned foods etc
- WHILE a diet high in fat and cholesterol can contribute to gallstone formation.
RISK FACTORS OF KIDNEY STONES AND GALL STONES
- People that have a family history of kidney stones and who are middle aged adults are at higher risks of developing kidney stones
- WHILE adults over 40, especially women and those who are overweight are at higher risks of developing gallstones
TREATMENT/MANAGEMENT OF KIDNEY STONES AND GALL STONES
- Kidney stones can be treated by removing the stones or adhering to a diet that controls the intake of the type of stone formed
- Gallstones can be treated by removing the gall bladder unlike kidney stones also and a diet with controlled cholesterol and low fat.
PREVENTION OF GALLSTONES AND KIDNEYSTONES
- To prevent gallstones, while trying to lose weight, make sure to do it slowly and correctly. Don’t skip meals and exercise regularly.
- Careful with the use of birth control pills to prevent gallstones
- Kidney stones can be prevented in a very easy way: just drink lots of water and maintain a healthy fluid level every day
If you’re experiencing any of these symptoms mentioned above, it is very important you contact health care givers and professionals so they could help treat whichever stone it may be.
SOURCES:
- https://www.adventhealth.com/hospital/adventhealth-orlando/blog/gallstones-vs-kidney-stones-how-similar-are-they#:~:text=A%20kidney%20stone%20is%20a,large%20as%20a%20golf%20ball.
- https://health.clevelandclinic.org/whats-the-difference-between-gallbladder-and-kidney-stones/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7311631/
- Quantitative analysis of gallstones using laser-induced breakdown spectroscopy.
Singh VK, Singh V, Rai AK, Thakur SN, Rai PK, Singh JP
Appl Opt. 2008 Nov 1; 47(31):G38-47.








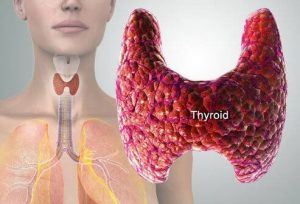

 Generally, one major factor considered to affect fertility is age. As you grow older, your organs, hormones and system seem to deteriorate.
Generally, one major factor considered to affect fertility is age. As you grow older, your organs, hormones and system seem to deteriorate.








 So many times we tend to eat when we’re not hungry due to emotional related issues.
So many times we tend to eat when we’re not hungry due to emotional related issues.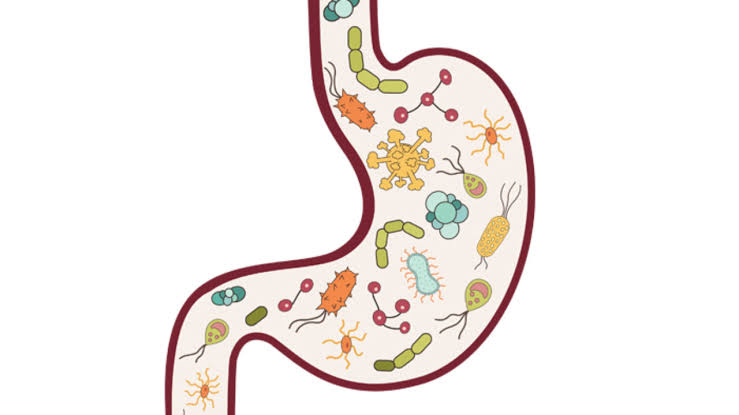
 The talk about gut health and hormones isn’t yet hitting the internet as it should. Rather, everyone is more concerned about their shape and the size of their belly. Your gut and hormones are intrinsically connected and affect your health in ways you can’t imagine.
The talk about gut health and hormones isn’t yet hitting the internet as it should. Rather, everyone is more concerned about their shape and the size of their belly. Your gut and hormones are intrinsically connected and affect your health in ways you can’t imagine.
