STRESS IN ITSELF
The word stress is quite a complex phenomenon with individualistic stress levels.
Stress is the body’s way to respond to triggering events that the brain goes through. It might be emotional, biological or physical response and might vary from individual to individual depending on the environmental and genetic factors involved.
When stress levels are low, the body is often in a state of homeostasis: All body systems are operating smoothly to maintain equilibrium.
POSSIBLE TRIGGERS
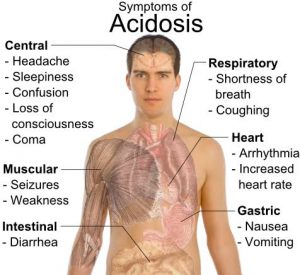
According to a research: Stressors trigger a “crisis-mode” physiological response, a physiological response which the body attempts to return to homeostasis by means of an adaptive response. The internal fight to restore homeostasis in the face of a stressor is known as the general adaptation syndrome, or GAS. The GAS has three distinct phases: alarm, resistance, and exhaustion. This leads to various physiological changes in the body. Stress is often described as a “disease of prolonged arousal” that leads to a cascade of negative health effects whose likelihood increases with on-going stress. Nearly all body systems become potential targets, and the long-term effects may be devastating.
Your stress levels when not adequately managed, could interfere with your medication and diet
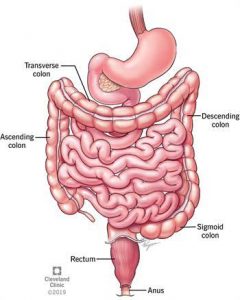
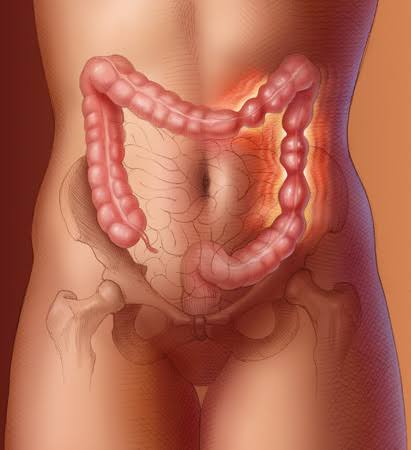
IRRITABLE BOWEL SYNDROME
On the other hand, Irritable bowel syndrome is your guts response to extreme stress levels
Triggers that easily affect the gut in IBS are sometimes perceived as psychological stress (loss of job, money, spouse), physical, physiological stress (diet, hormonal changes).
IBS can result from a very intricate biological interaction between the brain and the gut – this is why addressing psychological and emotional stressors that may be associated with IBS symptoms is the first step in understanding IBS triggers. Not all people with IBS have symptoms of psychological distress, but for those who do, stress management techniques become critical in managing IBS symptoms.
Another possible could be food anxiety (orthorexia), where one always gets worried about what to eat, how the food was prepared, the source and so on. Anxiety might precipitate IBS symptoms and not even the food itself.
STRESS MANAGEMENT TECHNIQUES AND DIETARY APPROACHES
Managing stress sometimes involves some self-care techniques which might include:
• Guided meditation
• Reading
• Knitting or needlework
• Bubble baths
• Exercise
• Listening to music
• Taking a stroll
It’s very important to note that everyone’s coping mechanism or stress management techniques are different. But it’s important to add these techniques to your daily routines.
DIETARY APPROACH
Role of specific nutrient in regulation of food intake, in the maintenance of homeostatic mechanisms and emotional processes is very dense. Serotonin (5-hydroxytryptamin or 5-HT) is synthesized from the dietary amino-acid tryptophan (TRP). Likewise, tyrosine is a precursor of noradrenaline (NA). Psychosocial and physical stress increases the rate of release of noradrenaline (NA) in both the periphery and the central nervous system hence more protein especially tyrosine is required. Likewise various other nutrients are required to reduce the levels of the stress chemicals (cortisol and adrenaline) that activate fight and flight response in the body.
Nutrients which includes vitamin C, vitamin B, tryptophan, threonine, magnesium, phenylalanine all have roles to play in helping individuals reduce stress levels and they could be found in grains, pulses, legumes and vegetables.
CONCLUSION
Stress management is different for everyone. It’s important to seek a therapist and medical care if your stress levels are extreme. For IBS patients, a change of lifestyle would suffice to manage symptoms.






 It’s obvious everyone wants to know if any dietary approaches or particular types of food could help prevent or even manage the incidence of the very dreaded COVID19.
It’s obvious everyone wants to know if any dietary approaches or particular types of food could help prevent or even manage the incidence of the very dreaded COVID19.

 Have you ever had a disruption in your bowels after taking a food you knew you shouldn’t have?
Have you ever had a disruption in your bowels after taking a food you knew you shouldn’t have? 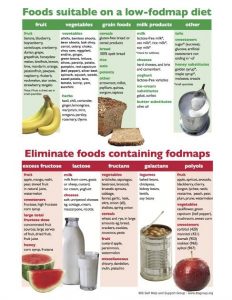

 Constipation is broadly defined as an unsatisfactory defecation characterized by infrequent stools, difficult stool passage or both.
Constipation is broadly defined as an unsatisfactory defecation characterized by infrequent stools, difficult stool passage or both.