Where the Science Aligns—and Where Concerns Remain
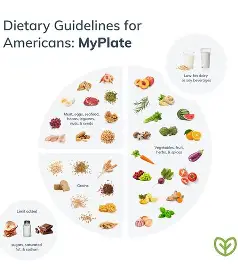
The Academy of Nutrition and Dietetics has formally acknowledged the release of the Dietary Guidelines for Americans (DGAs), 2025–2030, a document that shapes nutrition policy, federal food programs, clinical counseling, and public understanding of healthy eating for the next five years. As with previous editions, many of the recommendations are grounded in well-established nutrition science. However, the newly released food pyramids and accompanying guidance also raise several important concerns that warrant careful scrutiny.
This critique expands on the Academy’s position, highlighting both areas of alignment and points where the guidelines appear inconsistent with the current body of evidence or present challenges for practical implementation.
What the Academy Supports
1. Emphasis on Nutrient-Dense Foods
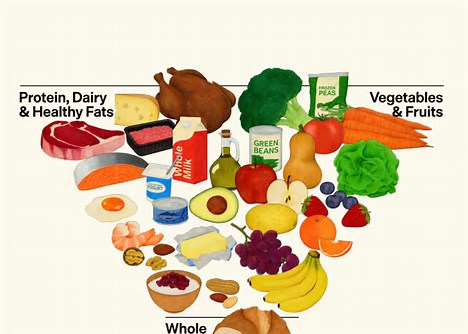
The Academy supports the continued focus on nutrient-dense foods, including fruits, vegetables, whole grains, legumes, nuts, and seeds. These foods are consistently associated with improved cardiometabolic health, reduced chronic disease risk, and better overall diet quality. Their prominent placement in the 2025–2030 food pyramids reinforces long-standing evidence that plant-forward eating patterns are beneficial across the lifespan.
2. Limiting Highly Processed Foods and Added Sugars
Another positive aspect of the DGAs is the recommendation to limit ultra-processed foods and added sugars. Excess intake of added sugars has been linked to obesity, type 2 diabetes, cardiovascular disease, and dental caries. Encouraging Americans to reduce sugar-sweetened beverages, refined snacks, and desserts aligns with decades of public health research and previous guideline iterations.
3. Saturated Fat Cap Remains at ≤10% of Total Calories
The Academy supports maintaining the long-standing recommendation that no more than 10% of total daily calories come from saturated fat, while encouraging the replacement of saturated fats with unsaturated fats such as those found in olive oil, canola oil, avocados, nuts, seeds, and fatty fish. This approach is supported by strong evidence demonstrating improvements in lipid profiles and reduced cardiovascular disease risk when saturated fat is replaced—not merely reduced.
4. Greater Attention to Fiber and Gut Health
The increased emphasis on dietary fiber and microbiome health reflects emerging science linking fiber-rich diets to improved glycemic control, cholesterol reduction, gut integrity, immune function, and potential mental health benefits. Highlighting whole plant foods as key fiber sources is a welcome and evidence-based advancement.
Where the Academy Has Concerns
1. Mixed Messaging on Saturated Fat
Despite maintaining the ≤10% saturated fat limit, the 2025–2030 DGAs place visible emphasis on foods such as butter, beef tallow, red meat, and full-fat dairy within the food pyramids. This creates a fundamental inconsistency.
The preponderance of evidence shows that these foods are significant sources of saturated fat, which is associated with increased LDL cholesterol and higher cardiovascular disease risk. While these foods can technically fit into a diet below the 10% threshold, their visual and narrative prominence risks confusing consumers and may undermine efforts to reduce saturated fat intake at the population level—particularly in communities already exceeding recommended limits.
2. Limited Consideration for Dairy Alternatives and Dietary Diversity
The new guidelines continue to center dairy as a core food group, with insufficient attention to individuals who cannot or choose not to consume dairy due to lactose intolerance, milk protein allergy, cultural dietary patterns, ethical preferences, or plant-based eating choices.

Millions of Americans; particularly individuals of African, Asian, Hispanic, and Indigenous descent, experience lactose intolerance. Failing to equally emphasize nutritionally adequate non-dairy alternatives (such as fortified soy beverages or other calcium- and vitamin D–rich foods) may reduce the inclusivity and applicability of the guidelines.
3. Caution Around Low-Calorie Non-Nutritive Sweeteners
The DGAs emphasize moderation and caution regarding low-calorie non-nutritive sweeteners, despite the fact that the current evidence base generally supports their safety when consumed within established acceptable daily intake levels.
While ongoing research is appropriate, framing these sweeteners as a concern without equally emphasizing their potential role in reducing added sugar intake may inadvertently discourage their appropriate use; particularly for individuals with diabetes or those working to reduce caloric intake.
4. Overgeneralization of Concerns About Synthetic Food Dyes
Consistent with the Academy’s Nutrition Fact Check, the evidence suggests that a small subset of children may be sensitive to certain synthetic food dyes, particularly in relation to attention or behavioral outcomes. However, the overall findings remain inconsistent, and causality has not been firmly established.
The DGAs’ tone risks overstating the evidence, potentially fueling unnecessary fear or confusion among consumers. More nuanced language acknowledging the limited and mixed nature of current research—while calling for further study—would better reflect scientific consensus.
Implications for Public Health and Practice
“Some of the recommendations in the DGAs are not aligned with the current body of evidence and will create challenges for implementation, particularly across federal nutrition programs that serve millions of Americans,” said Deanne Brandstetter, President of the Academy of Nutrition and Dietetics.
“Registered dietitian nutritionists and nutrition and dietetics technicians, registered, play a critical role in applying the DGAs in ways that protect public health and meet the needs of a broad spectrum of populations. However, elements of this version of the guidelines will make that work difficult.”
This concern is particularly relevant for programs such as school meals, WIC, SNAP-Ed, and older adult nutrition services, where clarity, consistency, and evidence alignment are essential for effective implementation.
Health Implications of the 2025–2030 Food Pyramids
Beyond conceptual inconsistencies, the structure and emphasis of the new food pyramids may have real clinical implications for common chronic and diet-related conditions. Registered dietitians working in clinical, community, and federal nutrition programs must be particularly attentive to these downstream effects.
1. Constipation and Gastrointestinal Health
The DGAs appropriately emphasize fiber; however, the visual elevation of animal-based fats and lower-fiber foods (e.g., butter, tallow, red meat, full-fat dairy) risks crowding out fiber-rich plant foods in real-world eating patterns.
Low fiber intake remains widespread in the U.S., with most adults consuming less than half of recommended fiber intakes. Diets higher in saturated fat and animal products and lower in fruits, vegetables, legumes, and whole grains are associated with slower colonic transit time and increased constipation risk.

Implication:
If consumers interpret the pyramid as endorsing frequent intake of animal fats without equal emphasis on fiber targets (25–38 g/day), constipation prevalence, already high among older adults, children, and individuals with limited food access may worsen.
2. Gout and Hyperuricemia
The increased normalization of red meat and animal fats in the pyramid raises concern for individuals at risk of gout and hyperuricemia. Red meat and certain animal products are high in purines, which metabolize into uric acid.
Multiple studies show that plant-forward diets and lower intake of red and processed meats are associated with reduced gout risk, while saturated fat intake may impair renal uric acid excretion.
Implication:
Without clearer guidance, individuals with gout may misinterpret the pyramid as supportive of dietary patterns that increase flare frequency and medication dependence, rather than preventive nutrition therapy.
3. Kidney Disease (CKD)
For individuals with chronic kidney disease, dietary guidance must carefully balance protein source, saturated fat, sodium, phosphorus, and fiber. The pyramid’s emphasis on animal-based fats and proteins raises concern, as these foods are associated with:
- Increased dietary acid load
- Higher phosphorus bioavailability, which may be a concern with ESRD patients.
- Greater cardiovascular risk in CKD populations
Plant-based and plant-dominant diets have been shown to slow CKD progression, improve metabolic parameters, and reduce mortality risk.
Implication:
The pyramid may complicate nutrition education for CKD patients by visually prioritizing foods that conflict with renal-protective dietary patterns, especially in dialysis and pre-dialysis populations.
4. Cardiovascular Disease (CVD)
Cardiovascular disease remains the leading cause of death in the United States, making dietary messaging around saturated fat critically important. While the DGAs retain the ≤10% saturated fat limit, the visual and narrative prominence of butter, tallow, red meat, and full-fat dairy undermines decades of evidence linking saturated fat replacement—not moderation alone—to improved cardiovascular outcomes.
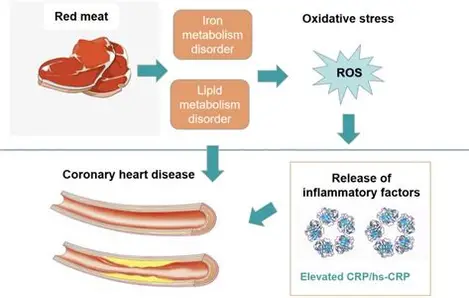
Implication:
Mixed messaging may lead consumers to underestimate the cardiovascular impact of saturated fat, potentially increasing LDL cholesterol levels at a population level—particularly among individuals already at high cardiometabolic risk.
5. The Place Given to Whole Grains on the Pyramids’ Scheme:
Whole grains have been long been established as healthy sources of carbohydrates, which is the body’s preferred fuel source. Whole grains are high in fiber, b-vitamins and minerals and are a preferred for diabetic patients, children, and the general population. The placing of this food group on the pyramid suggests that it should be eaten as little as possible, even though the evidence states that the average person needs between 45-65% of energy from carbohydrate sources.
Implications:
There is a possibility that these guidelines could increase risk of ketoacidosis, especially in diabetic patients. Furthermore, unless a person is a vegan/vegetarian, on a keto diet or on a carnivorous diet, there is simply no evidence base for this guideline.
Overall Public Health Considerations
Taken together, these implications suggest that the 2025–2030 food pyramids may inadvertently promote dietary patterns that:
- Worsen constipation through insufficient fiber displacement
- Increase gout flare risk via higher purine and saturated fat intake
- Complicate kidney disease management
- Undermine cardiovascular disease prevention efforts
For federal nutrition programs, clinical settings, and community education, this creates added burden for registered dietitians, who must actively reinterpret and contextualize the pyramid to align recommendations with evidence-based medical nutrition therapy.
Closing Perspective
While the Dietary Guidelines for Americans remain an essential public health tool, their effectiveness depends on clarity, consistency, and inclusivity. As nutrition science continues to evolve, visual models such as food pyramids must accurately reflect not only theoretical nutrient targets, but also the real-world health consequences of dietary patterns—especially for populations living with chronic disease.
Registered dietitian nutritionists will continue to play a critical role in translating these guidelines into practical, individualized, and protective nutrition care—but doing so should not require correcting the very framework meant to guide the public.