Ever wondered if any of your internal organs could affect your weight? Maybe due to its overactive nature or underactive nature?
Well, it is actually possible for an organ to affect your metabolism, growth and weight patterns and that organ is the thyroid.
Globally, 1.6 billion people are currently at risk of developing thyroid related diseases.
In this write-up, we’re going to see how the thyroid affects weight, for those who want to gain weight or lose it, if your thyroids are mal-functional, then you might just experience some difficulties with your weight.
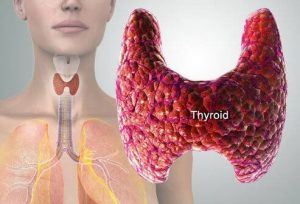
WHAT IS THE THYROID?
The thyroid gland looks like a butterfly and is located at the front of the neck right below the voice box (larynx).
The thyroid is small, but functions and affects all other organs in the body. It is involved in the regulation of fat and carbohydrate metabolism, respiration, body temperature, brain development, cholesterol levels, the heart and nervous system, blood calcium levels, menstrual cycles, skin integrity, and more.
WHAT IS THE IMPORTANCE OF THE THYROIDS?
The thyroid controls almost every major metabolic function in the body.
The hormones present in the thyroid glands are responsible for the regulation of the metabolic rate of all cells, as well as the processes of growth of cells, tissue differentiation, and reproductive function.
These hormones are also necessary for (and promote) protein metabolism when enough carbohydrates and fats are available.
When the amount of thyroid hormones is excessive or when energy from food is deficient, thyroid hormones (T3 and T4) promote protein breakdown. This processes in turn totally affects weight management.
WHY AM I FINDING IT DIFFICULT TO LOSE/GAIN WEIGHT
HYPOTHYROIDISM
It would be difficult for you to lose weight if you have the condition called hypothyroidism, or underactive thyroid.
Hypothyroidism is usually caused by an autoimmune response known as Hashimoto’s disease (a condition in which your immune system attacks your thyroid) or autoimmune thyroiditis (inflamed thyroids).
What happens in this disease is that your body mistakenly sees its own tissues as an invader and starts fighting against it. This process prevents the thyroid from releasing adequate hormones for the proper functioning of the body.
The lack of these hormones can slow down metabolism and cause weight gain, fatigue, dry skin and hair, and difficulty concentrating. Hypothyroidism affects women more than it affects men and is common in middle aged people. Also, women may also experience thyroid inflammation after pregnancy.
Some symptoms associated with hypothyroidism includes:
• tiredness, fatigue, lethargy
• depression and losing interest in normal activities
• forgetfulness
• dry hair and skin
• puffy face
• slow heart rate
• intolerance to cold
• constipation
• brittle nails
• muscle cramping
• changes in menstrual cycle
HYPERTHYROIDISM
A very common condition related with thyroid is hyperthyroidism or overactive thyroid gland. Hyperthyroidism is caused by an autoimmune response of the body in the form of Graves’ disease.
In Graves’ disease, the body produces too much of thyroid hormones and makes it seems like your body is revving so fast in response to these hormones.
This could also lead to weight loss, high blood pressure, and a rapid heartbeat. Graves’ disease also disproportionately affects women and typically presents before the age of 40.
Hyperthyroidism as an autoimmune diseases and have strong genetic links which are also associated with other autoimmune diseases as type 1 diabetes, rheumatoid arthritis, lupus and celiac disease.
The most common symptoms associated with hyperthyroidism includes:
• racing heart and palpitations
• trouble sleeping
• tremor and nervousness
• weight loss
• hair loss
• muscle aches and weakness
• diarrhea and over-active digestive system
• sweating and trouble tolerating heat
• exophthalmos (bulging eyes)
A goitre is the most common and evident symptom of chronic hypothyroidism. Some might have it, but not all.
Also, chronic or severe disease can manifest with dull facial expression, drooping eyelids, hoarse speech, thinning or dry and brittle hair, dry skin, myxedema (swelling of the skin and soft tissues), menstrual disorders, constipation, depression, anemia.
HOW DO I KNOW IF MY THYROID IS UNDERACTIVE/OVERACTIVE?
You can go for a thyroid function screening if you’re up to 40. A blood test is used to measure thyroid stimulating hormone (TSH).
WHAT ARE THE RISK FACTORS?
Gender. Majorly occur in women, especially those who had small weight at birth
Age.
Risk of hypothyroidism increases with age.
Genetics.
Psychological stress
Smoking
Iodine: excess dietary iodine intake and iodine-rich medication (amiodarone) may lead to hyperthyroidism.
IS HYPOTHYROIDISM/HYPERTHYROIDISM TREATABLE?
Yes it can’t! It can be treated medically by a hormone replacement therapy, administering oral thyroid hormones, and addressing iodine deficiency with potassium iodide.
CAN I STILL MANAGE MY WEIGHT WHILE WITH A DYSFUNCTIONAL THROID HORMONE?
Certainly you can! With the right approach, and evaluation of your hormones by specialists, also treating every imbalance, you can still lose or gain weight. Knowing the right type of dietary choices, the foods allowed and the foods to avoid makes it easy to lose weight.
A dietitian would help calculate your caloric needs and place you on a sustainable dietary pattern to help achieve your goals with your hormone therapy and exercise regimen.
Foods to avoid for hypothyroidism includes:
– refined carbohydrates and caffeine
– energy bars and genetically modified organisms (GMO) foods
– gluten-containing foods, such as wheat, rye and oats
– cruciferous vegetables like broccoli and kale.
– Soy and millet
Foods to include in hypothyroidism:
-vitamin B12 food sources like sardines, salmon, organ meats such as liver, muscle meat, and dairy
– foods rich in iodine like seaweed, iodized salt,
– Whole grains
– Legumes, eggs (especially egg white), nuts, nut butter
– Oily fish, flaxseeds, extra virgin olive oil and avocados will help balance your lipid
-brazil nuts, crabs and tuna fish which contain selenium
– incorporate healthy bacteria (probiotics) from pap, yoghurt. Kimchi and sauekrat
Foods to include in hyperthyroidism includes:
• non-iodized salt
• coffee or tea (without milk or dairy- or soy-based creamers)
• egg whites
• fresh or canned fruit
• unsalted nuts and nut butters
• homemade bread or breads made without salt, dairy, and eggs
• popcorn with non-iodized salt
• oats
• potatoes
• honey
• maple syrup
• Cuciferous vegetables might reduce how your body uses iodine and they include: bamboo shoots, bok choy, broccoli, Brussels sprouts, cassava, cauliflower, collard greens, kale, mustard, rutabaga
It is important to do away with the following seafood and seafood additives:
• fish
• seaweed
• prawns
• crabs
• lobster
• sushi
• carrageen
• agar-agar
• algae
• alginate
• nori
• kelp
Other foods that contain iodine includes:
• milk and dairy
• cheese
• egg yolks
• iodized salt
• iodized water
• some food colorings
Furthermore, foods that contain gluten, soy and caffeine should be avoided as they cause inflammation and can interfere with hyperthyroidism treatments.
It’s also important to note that, following a strict exercise regimen with your eating pattern is important. People with hypothyroidism would gain from lifting weights and dumb bells, and strength training.
DO I NEED TO GO ON A SPECIAL TYPE OF DIET?
One of the major concern in managing hashimoto’s disease is to look for a suitable type of diet to help manage and relieve symptoms. Hashimoto disease (hypothyroidism) is an auto-immune disease (ATD), so is gluten sensitivity and gluten intolerance. Research has shown the possibilities of using a gluten free diet in managing hashimoto’s disease as it helps to reduce the amount of thyroid antibodies.
A gluten diet involves the elimination of some certain types of foods that contain the protein gluten. Foods include wheat and its derivatives, bran and rye. This foods most times are re-introduced after symptoms has been optimally managed.
FOOD SUPPLEMENST AND INTERACTIONS
People with hashimoto’s are likely to de deficient in certain nutrients like vitamin B12 and vitamin D and would gain from supplementing with these nutrients.
Also, some anti-inflammatory supplements like selenium, fish oil, magnesium and zinc would also be beneficial to people with hashimoto’s as they help improve thyroid functions, reduce inflammation and improve overall health.
Remember that supplements are not meant to replace a nutrient dense and healthy diet.
For those on thyroid medications, it is important to note their interactions with some nutrients. Calcium supplements and chromium picolinate (used in weight loss and glucose control) both interfere with proper absorption of thyroid medications.
They should be both taken 4 hours apart from the time of administering thyroid medications as both can’ be stopped but are important in individuals with poor thyroid functions.
SUMMARY AND RECOMMENDATIONS
– Stay active
– Get rest when you’re tired. Don’t push it
– Stay hydrated always
– Stay away from caffeine and alcohol as much as you can
– Try yoga if you can
– Spend time outside
– Engage in stress reducing activities when you can.
SOURCES
1. Mahan LK & Escott-Stump S. Eds. Krause’s Food, Nutrition, & Diet Therapy. 11th ed. Saunders Publishing, Philadelphia, PA. 2004.
2. Beers MH, Berkow R eds. Merck Manual. 17th ed. Merck Research Laboratories. Whitehouse Station, NJ. 1999.
3. Teas J, et al. Seaweed and soy: companion foods in Asian cuisine and their effects on thyroid function in American women. J Med Food 2007;10:90-100.
4. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160(4):526-534.
5. Graves’ Disease. Bethesda, MD: National Endocrine and Metabolic Diseases Information Service, US Dept of Health and Human Services; 2008. NIH Publication No. 08-6217.
6. Biondi B, Klein I. Hypothyroidism as a risk factor for cardiovascular disease. Endocrine. 2004;24(1):1-13.
7. Duntas LH, Brenta G. The effect of thyroid disorders on lipid levels and metabolism. Med Clin North Am. 2012;96(2):269-281.
8. Dean S. Medical nutrition therapy for thyroid and related disorders. In: Mahan KL, Escott-Stump S, eds. Krause’s Food, Nutrition, & Diet Therapy. 13th ed. Philadelphia, PA: Saunders; 2008: 711-724.
9.https://www.medicinenet.com/cancer_101_pictures_slideshow/article.htm
10.https://www.healthline.com/health/hyperthyroidism-diet#takeaway


