The internet has so many people jumping on different products with bogus health claims making them look like pixie dust.
Apple cider vinegar is one of such products with so many purported health benefits. Now this doesn’t mean that apple cider vinegar is pixie dust or adder poison
Apple cider vinegar has some proven benefits and we’ll look into those benefits and limitations in this write up.
How Apple Cider Vinegar Is Made
Vinegar comes from a French word ‘vin aigre’, meaning sour wine. Apple cider vinegar is gotten from a process of ‘controlled spoilage’.
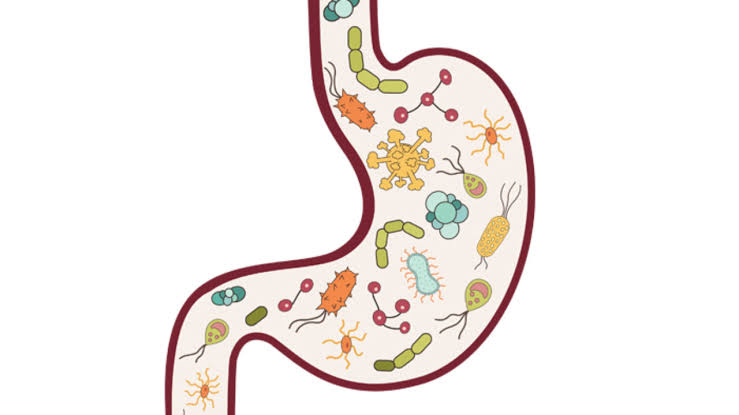
The sugars in apple is digested by yeast thereby converting it into alcohol. Then a bacteria, acetobacter converts the alcohol into acetic acid which gives it a sour taste.
The combination of yeast and bacteria (mother) acts as a probiotic.
The profile of apple cider vinegar which contains probiotics, acetic acid and other nutrients surely provides certain health benefits to the consumer:
CLAIMS
1. Apple cider may help with blood sugar control: the exact mechanism behind this is not really known, but some studies suggests suppression of disaccharidase activity, delayed gastric emptying, enhanced glucose uptake in the periphery and conversion to glycogen, and increased satiety. Some studies showed how taking in 20g of apple cider vinegar 30-60mins significantly lowered post pandral glucose levels.
Another study showed that vinegar does not act to decrease glycaemia by interference with enteral carbohydrate absorption.
In all, apple cider vinegar does not cure diabetes and cannot take the place of medication and dietary aides to manage diabetes but can be used alongside medications and diet to help in the management of diabetes.
2. Apple cider may help boost weightloss: some studies suggest that acetic acid can prevent fat deposition and improve metabolism. Taking 1-2 spoons of apple cider vinegar may help in modest weight loss by the mechanism mentioned above.
Studies also showed that participants ate a diet of 250 lesser than their normal daily requirements. Apple cider on its own won’t lead to weight loss, so don’t shove your meal plans and gym routines aside
3. Apple cider helps control blood pressure: no scientific claims to back this up on humans yet
4. Apple cider vinegar will not cure cancer
LIMITATIONS
– It can alter insulin levels thereby possibly leading to hypoglycaemia if taken in high does. Diabetic patients should be aware of this.
– It can damage the tooth enamel due to its high acidity. It should be diluted before consumption
– It might lower potassium levels. People with hypertension who are on diuretics should be careful with usage.
CONCLUSION
Apple cider vinegar is almost like any other over the counter supplement. It won’t replace healthy lifestyle.
SOURCES: 1.https://www.health.harvard.edu/blog/apple-cider-vinegar-diet-does-it-really-work-2018042513703
2. https://pubmed.ncbi.nlm.nih.gov/29091513/
3.https://www.uchicagomedicine.org/forefront/health-and-wellness-articles/debunking-the-health-benefits-of-apple-cider-vinegar







 The talk about gut health and hormones isn’t yet hitting the internet as it should. Rather, everyone is more concerned about their shape and the size of their belly. Your gut and hormones are intrinsically connected and affect your health in ways you can’t imagine.
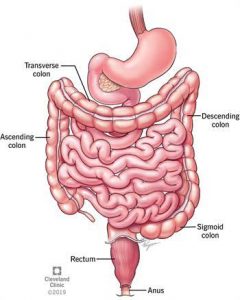
The talk about gut health and hormones isn’t yet hitting the internet as it should. Rather, everyone is more concerned about their shape and the size of their belly. Your gut and hormones are intrinsically connected and affect your health in ways you can’t imagine. Constipation is broadly defined as an unsatisfactory defecation characterized by infrequent stools, difficult stool passage or both.
Constipation is broadly defined as an unsatisfactory defecation characterized by infrequent stools, difficult stool passage or both.