OVERVIEW
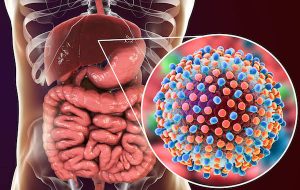
Everything you eat and drink has to go through your liver in order to change food substances into stored energy and chemicals which are necessary for life. Your liver makes nutrients available so your body can use them to build cells, give you energy, and maintain normal body functions.
The liver is responsible for:
– removing toxins from drugs and alcohol from the body
– metabolizing fat
– excretion of bilirubin (a product of broken-down red blood cells), cholesterol, hormones, and drugs
– breakdown of carbohydrates, fats, and proteins
– activation of enzymes, which are specialized proteins essential to body functions
– storage of glycogen (a form of sugar), minerals, and vitamins (A, D, E, and K)
– synthesis of blood proteins, such as albumin
– synthesis of clotting factors
HOW DIET AFFECTS THE LIVER
An unhealthy choice in diet can sometimes give the liver to much work to do thereby leading to a liver failure. If your diet provides too many calories, you will gain weight. Being overweight is linked to the buildup of fat in the liver, called “fatty liver.” Toxins, such as alcohol, damage the liver over time.
One very common liver disease (failure) is hepatitis.
Hepatitis refers to a common inflammation of the kidneys caused mostly by viral infections and other factors as toxins, auto immune diseases and alcohol.
There are different types of hepatitis and are all differentiated by Alphabets A-G.
According to the Centers for Disease Control and Prevention (CDC)Trusted Source, approximately 4.4 million Americans are currently living with chronic hepatitis B and C. Many more people don’t even know that they have hepatitis.
There are 5 types of viral infections with 5 distinct types of viruses:
Hepatitis A
Hepatitis A is caused by an infection with the hepatitis A virus (HAV). This type of hepatitis is most commonly transmitted by consuming food or water contaminated by feces from a person infected with hepatitis A.
Hepatitis B
Hepatitis B is transmitted through contact with infectious body fluids, such as blood, vaginal secretions, or semen, containing the hepatitis B virus (HBV). Injection drug use, having sex with an infected partner, or sharing razors with an infected person increase your risk of getting hepatitis B.
It’s estimated by the CDC that 1.2 million people in the United States and 350 million people worldwide live with this chronic disease.
Hepatitis C
Hepatitis C comes from the hepatitis C virus (HCV). Hepatitis C is transmitted through direct contact with infected body fluids, typically through injection drug use and sexual contact. HCV is among the most common bloodborne viral infections in the United States. Approximately 2.7-3.9 million people currently living with a chronic form of this infection.
Hepatitis D
Also called delta hepatitis, hepatitis D is a serious liver disease caused by the hepatitis D virus (HDV). HDV is contracted through direct contact with infected blood. Hepatitis D is a rare form of hepatitis that only occurs in conjunction with hepatitis B infection. The hepatitis D virus can’t multiply without the presence of hepatitis B. It’s very uncommon in the United States.
Hepatitis E
Hepatitis E is a waterborne disease caused by the hepatitis E virus (HEV). Hepatitis E is mainly found in areas with poor sanitation and typically results from ingesting fecal matter that contaminates the water supply. This disease is uncommon in the United States. However, cases of hepatitis E have been reported in the Middle East, Asia, Central America, and Africa, according to the CDC .
COMMON SYMPTOMS OF HEPATITIS
• fatigue
• flu-like symptoms
• dark urine
• pale stool
• abdominal pain
• loss of appetite
• unexplained weight loss
• yellow skin and eyes, which may be signs of jaundice
DIAGNOSIS OF HEPATITIS
Hepatitis can be diagnosed by liver function test, blood test, ultra sound, liver biopsy. The doctor always checks for risk before deciding what method to adopt in diagnosis.
TREATMENT OPTIONS FOR HEPATITIS
All types of hepatitis require either anti-viral vaccination, hydration if there is diarrhea (especially in type A), and nutrition.
Currently, there is no vaccination for Hepatitis C. Those that develop cirrhosis during the course of this would require a liver transplant.
Acute cases like Hepatitis E usually don’t require vaccination or treatment as they go on their own if the individual heeds to lifestyle modification by a professional.
RISK FACTORS
These include contact with an infected person (either living in close contact or sexual contact), poor hygiene, traveling to areas with inadequate sanitation, contaminated food (especially shellfish), and illicit drug use. Also, Patients with underlying liver disease (e.g., autoimmune hepatitis, hemochromatosis, Wilson’s disease, alpha-1 antitrypsin deficiency) are at increased risk of developing symptomatic hepatitis.
Alcohol use, smoking, HIV infection, and fatty liver are risk factors for progression of hepatitis.
NUTRITION AND HEPATITIS
Dietary management in hepatitis involves more of a lifestyle modification and hygienic approach.
Hygiene and sanitation: you should be careful of what you eat as a travller as you can pick up the virus from under cooked and contaminated foods. Make sure you heat food appropriately.
Avoiding contaminated shellfish and game meats.
Avoiding high-iron foods and iron supplements. Hepatitis C progression occurs in patients as a result of accelerated hepatic iron uptake and the oxidative stress caused by iron-catalyzed free radical production. Along with phlebotomy, a low-iron diet helps lower the risk for hepatocellular carcinoma (HCC) in these patients.
Nutritional supplementation may be required. Treatment with interferon (IFN) has shown to be very effective especially in Hep C patients. Research has it that it could help in weight reduction as it reduces appetite.
A low-fat, low-cholesterol diet may be helpful. Chronic hepatitis C (CHC) infection increases the risk for hepatic steatosis. A higher intake of dietary cholesterol contributes to this problem and is associated with the progression of hepatitis C-related liver disease. A dietary regimen that is reduced in fat (23% of calories) and cholesterol (185 mg/d) is adviced to help in the management of this Hepatitis.
Adequate vitamin D status. Vitamin D deficiency is common in patients with chronic liver disease, and these patients may have a reduced ability to convert vitamin D to its active form. An inverse relationship seems to exist between vitamin D concentrations and viral load in patients with CHC. Deficiency significantly lowers the chance for a sustained virological response to pegylated interferon and ribavirin, and vitamin D supplementation improves the probability of response to treatment.
Avoidance of extremes in B12 status. Adequate B12 status helps with clearance of hepatitis C from the circulation of infected patients. However, overly high serum B12 levels may also foster viral replication and are associated with concentrations of hepatitis C RNA levels.
Coffee consumption and chronic hepatitis C. Coffee consumption may be helpful, reducing oxidative DNA damage, increasing death of virus-infected cells, stabilizing chromosomes, and reducing fibrosis.
HOW HEPATITIS C AFFECTS DIET
If you have hepatitis, you usually don’t need a special diet. Just trying to eat healthy, maintain a healthy weight, and avoid alcohol is all that is needed. Its mostly lifestyle modification. Though, in severe cases, there might be nutrient restrictions especially fat restriction.
There are special cases, however, when hepatitis C can affect the diet:
• Patients with cirrhosis
As liver disease progresses, patients may lose their appetite and become so tired they have a hard time eating. They may become very thin and poorly nourished and be less able to fight off disease. They may need to limit salt in their diet to prevent their body from putting fluid into their legs and abdomen.
• Other medical conditions and diet
People who have other medical conditions may need other specific changes in their diet. Conditions that warrant specific dietary restrictions include high blood pressure, heart disease, diabetes mellitus, high cholesterol, celiac sprue or chronic kidney disease.
EATING TIPS
People with hepatitis C don’t need to follow a special “hepatitis C diet.” The advice that an average, healthy person gets will work just as well for people with hepatitis C, unless those people also have cirrhosis or another condition, such as diabetes, HIV, or kidney disease.
General dietary advice:
• Eat regular, balanced meals
• Maintain healthy calorie intake
• Eat whole-grain cereals, breads, and grains
• Eat lots of fruits and vegetables
• Get adequate protein
• Go easy on fatty, salty, and sugary foods
• Drink enough fluids
• Reach and maintain a healthy weight
Cautions:
• Avoid alcohol
• Be careful with dietary supplements
Herbal products
Just because something is “natural” doesn’t mean it is harmless. Certain herbs, including Kava-Kava and pennyroyal, can cause liver damage.
Endeavour to always talk to your doctor before taking megavitamin therapy, herbal products, or any other dietary supplement. Remember, your first concern should be safety.
SOURCE: https://nutritionguide.pcrm.org/nutritionguide/view/Nutrition_Guide_for_Clinicians/1342052/all/Viral_Hepatitis
https://www.hepatitis.va.gov/hcv/patient/diet/single-page.asp#:~:text=If%20you%20have%20hepatitis%2C%20you,is%20all%20that%20is%20needed.&text=As%20liver%20disease%20progresses%2C%20patients,have%20a%20hard%20time%20eating.

