Non Alcoholic Fatty Liver Disease: What you need to know
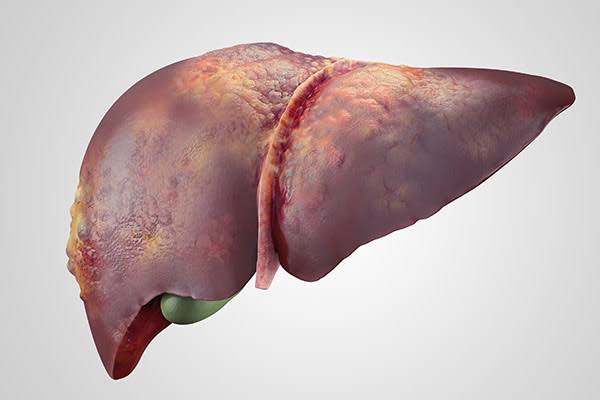
Your liver is your largest internal organ which is responsible for digestion, detoxification, and storage of energy.
A very little infection could lead to its damage if not treated properly.
The term ‘liver disease’ is a compendium of many different conditions including hepatitis, liver cancer, fatty liver disease and genetic conditions like hemochromatosis. Let’s delve a little bit into a disease that could be curbed nutritionally, especially one that affects about 25% of the world’s population (Non alcoholic fatty liver disease (NAFLD)
What is NAFLD & NASH?
Non-alcoholic fatty liver disease (NAFLD) is a condition in which fat is inappropriately stored in the cells of the liver. As the name implies, this particular type of fatty liver disease occurs in people who drink little/no alcohol – while there is also fatty liver that can result from excessive alcohol consumption. Often times, it’s not stereotypical, you may drink moderately, as well as have nutrition and lifestyle habits which can still contribute to fatty liver disease. Regardless of the cause, lifestyle changes are typically the first intervention.
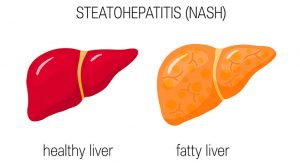
If left undiagnosed or untreated, having NAFLD could also increase a person’s risk of developing a more advanced form of liver disease, called non-alcoholic steatohepatitis (NASH). 30% of those with NAFLD progress to developing NASH. So, what’s the difference? In NAFLD, there are fatty deposits throughout the liver, but little to no inflammation or liver cell damage.
NASH on the other hand, is a form of NAFLD and is characterized by fatty deposits in the liver PLUS inflammation and liver cell damage, fibrosis (hardening of the liver) and can even lead to permanent scarring in the liver, called cirrhosis. In other words, it is more permanent and irreversible than normal NAFLD – but can still be managed with lifestyle, diet, and/or medications.
Why would someone who doesn’t consume excess alcohol still have fat deposits around their liver? There are a few risk factors that are associated with developing NAFLD and NASH including:
- Having characteristics of metabolic syndrome – this includes factors such as high blood pressure, high cholesterol, diabetes mellitus or insulin resistance, and large waist circumference
- Rapid weight loss may be due to a previous illness or stringent eating patterns
- Obesity
- Excessive intake of energy, in particular fat and sugar, and overall lack of balance in the diet
- Genetic risk factors
SYMPTOMS OF NAFLD?
One of the most challenging aspects of NAFLD and NASH is that they could be asymptomatic, particularly in the early stages in which many people get little to no symptoms at all. If individuals do present with symptoms, they generally experience one or more of the following things:
- Pain/discomfort in the upper right abdomen (where the liver is located)
- Fatigue
- Unexplained weight loss
- General feeling of unwell
“In the more extreme cases, where liver cirrhosis and scar tissue develop, people may experience fluid buildup called edema or ascites, and yellowing of the skin and eyes called jaundice”. However, this is unlikely to occur in the beginning stages of NAFLD and NASH.
“Because this condition is difficult to detect with physical symptoms, it is key to manage your health by seeing your doctor regularly and having routine blood work – usually annually or every couple of years unless you are at higher risk. This is especially important for anyone with a personal history or family history of liver issues, diabetes mellitus (particularly type 2), or any of the other risk factors listed above”.
How is NAFLD diagnosed?
Doctors use routine medical check-ups in detecting liver disease, which can involve physical examination, blood work, and imaging tests. In many cases, the first signs of NAFLD pop up in blood tests. Doctors will commonly include a check for liver enzyme levels including alanine aminotransferase (ALT) and aspartate aminotransferase (AST). If these are elevated, your doctor may want to investigate fatty liver disease.
Other tests for diagnosing NAFLD & NASH include imaging tests such as abdominal ultrasounds, fibro scans, and CT scans to view the liver and detect fatty tissue.
A combination of blood tests and imaging is typically enough to determine if someone has NAFLD, but your healthcare team may decide to do additional testing to identify the severity of your condition such as a liver biopsy or additional blood testing.
ARE THERE TREATMENT OPTIONS?
You have realized that drinking alcohol In moderation doesn’t stop you from developing NAFLD, so it’s wise to watch your lifestyle patterns to avoid developing this disease. Poorly managed fatty liver disease can ultimately lead to cirrhosis and increased risk of liver cancer.
Treatment of NAFLD involves a combination of lifestyle and medication management, although some people might not require pharmacotherapy to improve their liver function.
IS THERE NEED TO LOSE WEIGHT IF I HAVE NAFLD?
A vast majority of the recommendations that exist regarding nutrition for NAFLD are focused on reducing overall weight as a means for improving liver biomarkers. However, a systematic review from 2003 revealed that a vast majority of the studies that analyzed the connection between weight reduction and NAFLD had flawed methods, making it difficult to truly connect the dots between weight loss and NAFLD, predominantly because weight loss if often not permanent, and weight cycling appears to be a possible risk factor for worsening NAFLD and progression to NASH or cirrhosis.
As earlier stated, weight loss especially if rapidly chased, could lead to development and worsening of NAFLD . Pursuing weight loss does not always mean someone is healthy! If weight loss must be involved, it should be realistic and sustainable and not some type of “crash diet” lose 30kg in 3 weeks” type of diet.
DIETARY MANAGEMENT
There is no standard “NAFLD diet”, but there are some key dietary concepts that are linked to better outcomes in those with non-alcoholic fatty liver which includes :
- Reducing saturated fat intake – saturated fat is primarily found in animal products, particularly beef, pork, creamy sauces, cheese, and other high fat dairy. It is also in coconut and palm oil.
- Reducing intake of simple carbohydrates, especially fructose – high consumption of simple sugars such as those found in pop, juice, baked goods, candy and highly processed grains can contribute to excess fat being deposited in the liver. Avoiding these foods is recommended. Enjoy these foods occasionally and continue to eat natural sugars from fruits, vegetables, and dairy.
- Increasing consumption of unsaturated fats such as omega-3s – Omega-3 fatty acids have been shown to help with reducing inflammation and fat synthesis in the liver. Foods high in omega-3 fatty acids include fish (particularly salmon, trout, tuna, mackerel & sardines), nut, seeds, plant oils and fortified foods like omega-3 eggs.
- Increasing fibre consumption – getting enough fibre in the diet can actually help to reduce the amount of fat we uptake into our bloodstream and carry to the liver. Fibre, particularly soluble fibre, binds to fat in the digestive track and helps us to do away with it naturally. Yes sure- we poop it right out! Fibre also plays a key role in regulating blood sugars and gut health, both factors implicated in the development of NAFLD.
- Reducing or eliminating alcohol intake – like mentioned earlier, we often see those with moderate alcohol intake diagnosed with NAFLD. Alcohol is very hard on the liver, so reducing intake or entirely cutting it out is helpful.
- Exercise – staying active always is a key component of reducing fat deposits in the liver. If you think the gym is a scary place, then you can try dancing.
THINK MEDITERRANEAN!
To be on a safer path, following a Mediterranean-style eating plan with an emphasis on lots of plant-based foods (veggies, fruit, and whole grains) ,leaner cuts of meat like chicken, turkey, and fish. Alongside this, consuming 1-2 meatless meals that include pulses like beans, chickpeas, and lentils is a great way of displacing intake of foods higher in saturated fat, plus an excellent source of fibre which might range from fleshy fruits with pulps or leafy vegetables.
Working with a dietitian is also highly recommended if you have NAFLD, as each case is very unique and should be individualized.
Medications
“There are numerous drugs that have been studied for NAFLD – almost too many to count! Generally speaking, medications used for the treatment of NAFLD mainly target the underlying cause (or suspected cause) of NAFLD”. In particular, medications that aid in cholesterol reduction and blood sugar management are a mainstay of care for NAFLD.
SUMMARY
If you have been recently diagnosed with NAFLD, working with a dietitian to incorporate a balanced diet that will help to reduce fatty deposits in your liver is highly recommended!
Many health professionals would encourage weight loss to treat NAFLD. While this might sound appropriate, please remember that weight loss without a focus on sustainable behaviours and long-term health can actually worsen NAFLD, particularly rapid weight loss.
Sources: https://ignitenutrition.ca/blog/non-alcoholic-fatty-liver-disease-what-you-should-know/?utm_source=dlvr.it&utm_medium=twitter